Plantar fasciitis is a common condition which has various causes. It can occur in active individuals in which case the case may be more likely due to training overload, but also affects people with a sedentary lifestyle. It’s often triggered after a “spike” in walking or running +/- less than ideal foot wear that isn’t very supportive. Anecdotally I’ve heard a lot of patient histories reporting holidays in flip flops with a lot of walking that preceded the pain. Ugg boots have also made appearances in these stories!
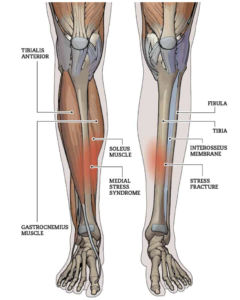
The exact cause of plantar fasciitis is poorly understood. It is thought to be an ‘overload’ ‘overuse’ ‘repetitive strain’ problem. The plantar fascia itself is a tough band of fibrous tissue that extends from the heel bone to the metatarsal bones of the foot. It supports the longitudinal arch and takes a lot of load during walking and running. While the term Plantar Fasciitis is most widely know it’s not thought be condition involving inflammation (aside from the very acute initial stages perhaps). It’s thought be more an overload leading to impaired load tolerance of the connective tissue.
Good news is there are lots of evidence-based treatments are available for plantar fasciitis and there’s around a 90% success rate with conservative management i.e. non invasive treatments (McPoil et al 2008).
1. Stretching exercises (Rathleff, 2014)
Regular stretching of the calf muscles and plantar fascia can help reduce pain and improve flexibility. Exercises such as toe stretches, calf stretches, and towel stretches are commonly recommended. The recommended hold time is 10secs for 10reps 3 x daily. If you struggle to get into this position you can try keeping the foot down and using a towel or a belt around the foot or placing the ball of your foot/toes up against a wall.
2. Strengthening exercises (Rathleff, 2014)
How does strengthening help? One theory is that it stimulates collagen synthesis which aids in normalising the plantar fascia structure and rebuilding it’s resiliency and ability to handle the strain that goes through it. Improvement in symptoms may come from improving ankle flexibility (limited ankle mobility is a known risk factor for the development of plantar fasciitis). Either way, there are two ways of going about this exercise program:
Source: Rathleff et al (2014) BJSM
Method 1) Structured
Tempo: (what pace to perform them) 3secs up, 2sec pause at the top and 3secs down
Reps/Sets/Load: (how many & how heavy)
Weeks 1-2 = 3×12 RM
Weeks 3-4 = 4×10 RM
Weeks 5-12 = 5×8 RM
*RM = a weight you can perform no more than the specified number of reps with
Frequency: Every other day
Duration: 12 weeks
Consistency: In the studies looking at the efficacy of these types of interventions, guess what one of the main determining factors is between those who do well and those that don’t? Adherence. Not a big surprise. If you do it, you will most likely succeed. If you don’t, you won’t.
Method 2) Self-dosed
If you’re not one for strict schedules or struggle to follow rigid plan like the one above, there’s good news! A study looking at self-dosed application of the strengthening shows similar success rates at 12-weeks (Riel et al, 2019)
The self-dose group were doing as many sets as they wanted with as heavy a load as possible (no heavier than 8RM i.e. a weight you can perform no more than 8 repetitions with).ks
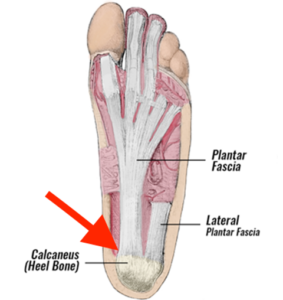
“Why the rolled up towel?” I hear you ask.
Good question. The theory is that incorporates the Windlass Mechanism:
Image source: Foot Injury Clinic Bondi Junction
The only issue I find in practice with using the rolled up towel is that it gets easily “smooshed” so you might want to consider something like the Fasciitis Fighter
3. Taping (Radford et al 2006)
What I can tell you anecdotally from experience when I’ve used taping with patients is this that I’ve had some success reinforcing the medial/inner arch. I use it sometimes as a trial test to see whether an orthotic might be worth giving a go. It simulates what an orthotic would essentially do and as the taping is tricky to apply yourself, if you feel better from it, it’s probably worth trying out some inserts to slot into your shoes. The proposed mechanism is that taping offloads the plantar fascia by mechanically altering foot posture and supporting the arch. This is a good option in the short term if it’s really sore to get the pain under control.
Image source: Radford et al (2006)
3. Orthotics / Heel Cups:
Shoe inserts like gel heel cups or orthotics can provide support, cushioning, and proper alignment for the foot. They help distribute pressure more evenly and relieve stress on the plantar fascia. Please remember to date there is no evidence showing that bespoke orthotics are superior to standard. So don’t spend an arm and a leg getting a special made orthotic unless you’ve at least tried the basics first.
The heel-cups I recommend are by Tuli’s HERE
Please make sure you choose appropriate size based on weight and shoe size for best results
If you find the heel cups are moving around too much another option are Heel Sleeves HERE
These are the orthotics I’ve found helpful HERE
4. Extracorporeal Shockwave Therapy (ESWT):
This involves delivering high-energy sound waves to the affected area to stimulate healing and reduce pain. Worth considering when other conservative treatments have failed at around the 4-6 week mark.
5. Corticosteroid injections:
The last resort. If you’ve tried all the above and you’re not feeling any better, this should be on the table for discussion from the 12 week mark. I would advise you don’t rush into this and talk through the benefits and risks with your health care provider. It’s certainly not a silver bullet and there are some risks involved, namely increased risk of plantar fascia rupture. You need to remember that whilst there may be some inflammation in acute cases of plantar fasciitis it’s generally considered to be more of a repetitive strain type condition that involves a weakening and disorganisation of the connective tissue. I’m using lay terms here to try and describe it, but the point is in you go in with an anti-inflammatory bazooka for a condition at a stage whether there isn’t presence of inflammation…
10. Weight management:
Obviously this isn’t something that is achievable quickly or going to give you immediate pain relief, but high BMI is research confirmed risk factor for developing plantar fasciitis (Van Leeuwen et al 2016). If you have high BMI (normal range between 18.5 – 24.9) once you’ve settled the pain you may want to consider developing a healthy weight-loss plan (check out my blog post on weight-loss ideas). Maintaining a healthy weight can help reduce the strain on the feet. Avoiding or modifying activities that exacerbate symptoms, such as excessive running or jumping, can also be beneficial.
That’s a Wrap!
So that’s it for now! A few honourable mentions I would mention anecdotally would be soft tissue massage through the calf and Achilles, theory being anatomically the plantar fascia shares a fascia connection with these structures. I’ve certainly had patients report relief from this even if it is just short-term. There are cupping techniques that can be used and I’ve played around with following courses that I’ve attended with some positive effects. I deliberately didn’t post the “rolling a ball or water bottle” here because everyone is already aware of that.
Good luck! And any questions feel free to reach out via the contact section.
Jay